43 Posts0.2k Comments
An autistic barbie that feels centered on autistic kids and that actually matters
Mattel has launched its first autistic Barbie, and what stands out to me is how clearly it’s designed with children in mind. Not to define autism by appearance, but to reflect some of the ways autistic kids experience, process, and communicate with the world around them. She has noise-canceling headphones, which instantly made sense to me. So many kids rely on them just to get through everyday environments. She’s holding a fidget spinner, something a lot of children use to regulate and stay grou

10
43 Posts0.2k Comments 155
7 Posts31 Comments

✈️✨ Autism-Friendly Travel Tool Alert! ✨✈️
I recently discovered Ella.kids, an incredible AI-powered app that can write custom social stories and create task cards or visual schedules for any situation you describe! This is a game changer for autistic travelers and families who want to prepare for new experiences. Whether it’s flying for the first time, going through airport security, or checking into a hotel, you can describe the situation and Ella.kids will build a personalized social story to help preview each step of the trip. 💡 Wha

40
7 Posts31 Comments 31
30 Posts54 Comments

What’s a weeknight meal you make so often you don’t even think about it anymore?
Here’s mine. I’ve made it so many times I don’t even follow a recipe anymore, I just know the order. It’s a classic American baked ziti that somehow ends up on our table at least twice a month. How it goes (no measuring, just vibes):1 lb ziti or penne1 lb ground beef or Italian sausage1 jar marinara sauce1 small onion, diced2 cloves garlic, mincedRicotta cheeseShredded mozzarellaA little ParmesanOlive oil, salt, pepperBoil the pasta in well-salted water and drain it a minute before it’s fully do
10
30 Posts54 Comments 54
31 Posts0.1k Comments

What level of effort are men actually expected to show?
This week, two women told me they weren’t sure if I was interested, which genuinely surprised me. From my perspective, I was consistent: replying, asking questions, remembering details, and suggesting we meet. One woman and I talked daily for about five weeks. I initiated most conversations and brought up meeting a few times, but it never really progressed unless I pushed. When I finally asked about the lack of initiative, she said she didn’t think I was that interested. Another woman asked if I
10
31 Posts0.1k Comments 104
26 Posts13 Comments
ExeKiller just dropped a new gameplay overview trailer 👀
If you’re into gritty post-apocalyptic shooters with a twist, this one might hit your radar. ExeKiller from indie dev Paradark Studio, is shaping up to be a retro-futuristic western-style FPS with choice-driven gameplay and survival elements set in a burned-out world where corporations rule and bounty hunters are the law (or lack thereof). The game doesn’t have a release date yet, but ExeKiller is still in development and available to wishlist on Steam. Trailer link: 🎮 https://youtu.be/dEeUzd4n

10
26 Posts13 Comments 13
3 Posts0 Comments

What is the Medicaid Waiver?
It is designed to allow individual with disabilities to receive long term care services in their home or community. It supports independent living and provides care that is tailored to their individual needs.
20
3 Posts0 Comments 0
26 Posts90 Comments

How a slight change in my sleep schedule can turn my night upside down
Some nights feel like my brain simply refuses to sleep because the world shifted, even just a little. I have profound autism, and for me, small changes aren’t small at all, they’re earthquakes. A bedtime ten minutes later than usual or a different room can leave me anxious, restless, and sometimes on the edge of a meltdown. Staying at a relative’s house is one of the hardest tests. The bed feels wrong, the sheets smell unfamiliar, the lights are brighter, and the room doesn’t smell like home. My

10
26 Posts90 Comments 90
26 Posts13 Comments

Thoughts on Netflix’s His & Hers?
Just watched His & Hers, the new Netflix thriller released last week starring Tessa Thompson and Jon Bernthal, based on the Alice Feeney novel. It follows an estranged couple a former TV journalist and a small-town detective who get pulled into the same murder case in their old hometown. The story jumps between perspectives, past and present, and leans hard into twists and unreliable narrators. Performances are solid but the show seems pretty divisive. Some people are calling it a fun, bingeable

10
26 Posts13 Comments 13
25 Posts13 Comments

Fashion feels different in 2026, curious if anyone else notices this
I’m noticing a shift in fashion lately, and I wanted to put it into words and see if it resonates with anyone here. Baggy jeans aren’t wrong. I still like them. But for me, they’re not doing the heavy lifting they used to. They feel more like background clothes now. That’s why I’ve been gravitating toward cigarette jeans they feel intentional, structured, and a little more grown-up. They make sense for where I’m heading in 2026. Clear lines, predictable fit, no guessing. I’m also finding myself

10
25 Posts13 Comments 13
27 Posts32 Comments
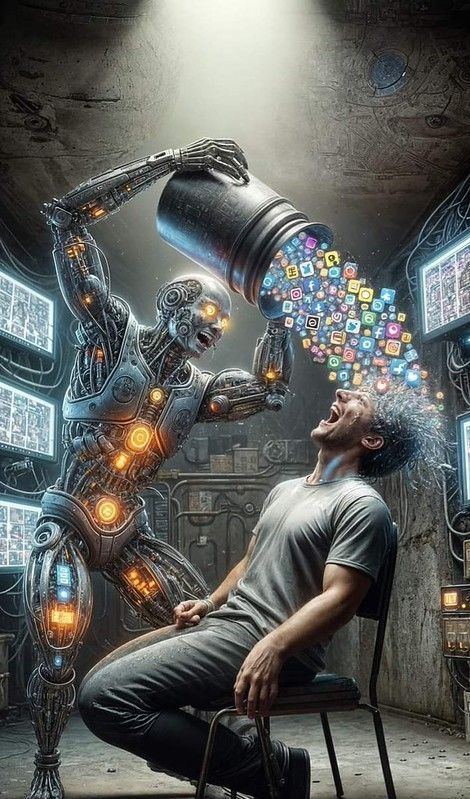
AI Is powerful but we need to teach our communities to spot fake content
I’ve been thinking a lot about how AI is changing the way we see the world for better and worse. People often talk about AI as this amazing tool that can do incredible things and it can. But we also need to be honest about the darker side of it. Recently, I saw examples that really alarmed me. Some folks on X were using AI tools like Grok to create explicit images. And even worse, there are AI-generated videos showing people crying in Venezuela after a fake arrest of President Nicolás Maduro by
10
27 Posts32 Comments 32